Sarah Jacobson Remembers her Father, Dave Jones 21 Apr 12:31 AM (7 days ago)
This is a guest post by Sarah Jacobson, who’s father Dave Jones was diagnosed with kidney cancer and passed away in March 2025.
My father Dave Jones was diagnosed with collecting duct renal cell carcinoma in March of 2024. He had a sister pass from pancreatic cancer several years ago and then a brother diagnosed with pancreatic cancer in early 2024. That led my dad to get screened for pancreatic cancer. His CT scan was negative for it, but it was found that he had stage 4 kidney cancer. He passed on March 4, 2025.
My dad ultimately passed from rare complications from one immunotherapy treatment. I hope these complications will be learned about more in the future.
My dad is an inspiration for so many reasons. His life wasn’t always easy. He and his siblings ended up in the foster care system when my dad was only 6. He was taken in by a lovely family and was cherished after that.
In 1977 he decided he wanted to start his own plumbing business. He started it in his garage with one employee. Now, in 2025, the business has over 600 employees. He retired about 10 years ago and passed the business along to his children. He and my mom, his wife of 52 years, were living their best life at their lake house and wintering in Alabama.
Dave was involved with several organizations over the years. A firefighter, a Mason – he valued the brotherhood of being a Mason. He also was involved in many plumbing and heating associations.
Dave was an avid hunter, often taking trips to Alaska and out West. It was a big passion for him.



However, his happiest moments were with his family. He was so proud of his three children and nine grandchildren. A real family man with family values. He was so loved and it showed through the very large turnout at his services.
While it was never spoken about due to my father being a pretty private man, I know the cancer diagnosis was very hard on him. It was very easy for me to read the room when he was around. I can say with certainty this man did not want to be sick, or pass away. It will always make me angry that this had to happen to him
I researched everything I could on his type of cancer. I wanted to be the best advocate for him that I possibly could. I followed his lab and scan results like a hawk, even looking up each and every word that I didn’t understand. We even took him to MD Anderson for a second opinion. No one prepared me for how hard it would be to watch my dad, the man who was always so strong, so smart, decline.
His death has taught me the importance of family, and the importance of cherishing the time that we all have on this earth – time is precious and a thief.
The post Sarah Jacobson Remembers her Father, Dave Jones appeared first on Kidney Cancer Association.
Recap – 2025 KCA regional Challenge: Austin 17 Apr 5:21 AM (11 days ago)
Team – 2025 KCA Regional Challenge: Austin
Team Captain – Annamaria Scaccia, 2-time cancer survivor and Member, KCA’s Patient & Caregiver Advisory Council
Location – Lake Pflugerville Park, Pflugerville, Texas
Date – April 12, 2025
Attendees: 11
Fundraising Goal – $3,000
Amount Raised – $3,284
Activity – 81-minute walk around Lake Pflugerville


Event Highlights – My favorite highlight was seeing everyone show up and stay fully engaged throughout the event. I let folks know they could walk at their own pace and didn’t have to stay together, but instead, we moved as one group and finished around the same time. That meant the world to me. It showed just how much everyone cared about the cause and wanted to be there.
Some participants brought their families, and they jumped in wholeheartedly. They wore orange, stuck with the walk, and brought this incredible energy that lifted the whole experience. At one point, strangers even stopped to ask what we were doing. Our banner and setup caught their attention, and it gave us a chance to talk about kidney cancer and why we were walking. It was such a powerful reminder that even a small group can make big waves.
What advice do you have for other event captains?
- Don’t go it alone. Build a small team. One of the best things you can do is form a committee. Whether it’s other survivors, friends, family, or coworkers, having a few people to help you plan, promote, and raise money makes the process way easier. You don’t have to do everything yourself.
- Ask for help early and often. Maybe you can’t find a venue. Maybe you aren’t sure how to get people to show up. If you’re stuck, reach out to KCA and let them know what you need. The same goes for your fellow hosts—don’t be afraid to ask for their opinions, to leverage their ideas, or to cross-promote your events. They all want your event to succeed and can often help more than you think.
- Keep the event simple and accessible. A 5K is a great format because it’s easy to organize, familiar to most people, and doesn’t require a ton of resources. You don’t have to come up with something brand new or out of the box.
- Reach out beyond your circle. Start with your own network but also connect with local community groups, small businesses, fitness clubs, or health organizations. You never know who might be willing to support the cause. People are often excited to get involved when you give them the chance.
- Start promoting early. Give yourself time to spread the word. Post on social, hang flyers in local cafes, send emails to friends and coworkers, and connect with community media. The earlier you start, the more chances you have to build excitement and get people to commit.
- Get creative with sponsorships. Sponsors don’t always have to contribute money. Local businesses can help in other ways too. A coffee shop might donate drinks, a gym might offer free passes as prizes, or a print shop might cover banners. In-kind donations like these can cut down your costs, so don’t be afraid to make the ask.
- I’d reach out to my doctors to promote the event in their offices. Another thing I didn’t think of at the time was asking my doctors if they would help promote the event in their offices. They’re already connected to the cancer community and could have helped spread the word to others who might be interested in getting involved.
Final Comments
This year, we put together a more intentional and engaging setup (shoutout to fellow REA host Lindsay Walker for the great idea to highlight survivor stories). We added a donation station and a large event banner, which grabbed the attention of folks out for a run on the lake trail. Many stopped to see what was going on, and we got to share more about kidney cancer, survivorship, and KCA’s mission. It was an effective way to raise awareness and make the cause more visible.
The post Recap – 2025 KCA regional Challenge: Austin appeared first on Kidney Cancer Association.
KCA Ambassador Featured on Cancer Interviews Podcast 16 Apr 6:10 AM (12 days ago)
In a new episode of the Cancer Interviews podcast, host and prostate cancer survivor Bruce Morton speaks with Kidney Cancer Association Ambassador Jeff Kallis about his journey with kidney cancer and how it led him to advocacy.
Jeff was diagnosed with stage 3 clear cell renal cell carcinoma in 2023. Since then, he’s not only navigated treatment and recovery, but found new purpose in supporting others. He’s become a passionate advocate for kidney cancer awareness and launched a kidney cancer and chronic kidney disease community at KidneyCouch.com.
In their conversation, Jeff and Bruce highlight the invaluable role the KCA plays in supporting patients and caregivers — offering trusted information, connecting others, and helping individuals feel empowered. They reflect on how KCA resources like educational materials, support groups, and advocacy opportunities, can truly make a difference in navigating the uncertainty of a cancer diagnosis.
Read more about Jeff:
The post KCA Ambassador Featured on Cancer Interviews Podcast appeared first on Kidney Cancer Association.
Three Special Lectures at 2025 IKCS: Europe 16 Apr 5:55 AM (12 days ago)
The 2025 International Kidney Cancer Symposium: Europe, taking place in Amsterdam on May 1-3, will feature three special lectures recognizing outstanding leaders in kidney cancer.

Dr. Michael Staehler
Dr. Michael Staehler will receive the KCA’s John Fitzpatrick Award recognizing excellence in urology care. Dr. Staehler is the founder and head of the Interdisciplinary Center for Renal Tumours at Ludwig-Maximilians University of Munich in Germany. It is the first multi-disciplinary cancer center for renal neoplasms in Germany certified by the German Cancer Society (DKG). Professor Staehler is also Head of the Urological Oncology Service for Advanced Genitourinary Cancer and Kidney Surgery. He is vice chairman of the Department of Urology of the University of Munich and heads the interdisciplinary tumor board on genitourinary cancer at the Comprehensive Cancer Center of the University of Munich. Dr. Staehler has supported with the Kidney Cancer Association over many years, including as a past chair of the IKCS: Europe scientific planning committee.

Dr. Tom Mitchell
Dr. Tom Mitchell will receive the Christopher G. Wood Rising Star Award, which recognizes talented young kidney cancer experts in honor of the KCA’s late Board Chair and friend, Dr. Christopher G. Wood. Dr. Mitchell is a Consultant Urologist at Addenbrooke’s Hospital. He is also the Research Group Leader of the Early Cancer Institute at the University of Cambridge, A Cancer Research UK Clinician Scientist Fellow, and in October 2024 was named the Krishnan-Ang Distinguished Group Leader of Cambridge’s Urological Malignancies Virtual Institute (UMVI).

Dr. Lisa Derosa
Dr. Lisa Derosa will give the 2025 IKCS: Europe Keynote Lecture discussing the Microbiome in Kidney Cancer. Dr. Derosa is a medical oncologist and head of The Clinicobiome Programme at the Institut Gustave Roussy in Paris, France.
The post Three Special Lectures at 2025 IKCS: Europe appeared first on Kidney Cancer Association.
Kidney Cancer Research Updates for the Entire Clinical Team 1 Apr 12:37 PM (26 days ago)
A significant amount of new, practice-changing information about kidney cancer has been published and presented over the last 18 months. It can be challenging for nurses, pharmacists, nurse practitioners, physician assistants, and other clinicians to keep up with every update. No worries: a few members of the Kidney Cancer Association’s Clinical Advisory Board (CAB) conducted reviews for you and provided summaries. Read on to learn more!
- Study design: Phase 3, randomized, double-blinded trial
- Patient population: previously untreated, IMDC intermediate or poor risk advanced renal cell carcinoma (RCC)
- Endpoints:
- Primary: Progression Free Survival (PFS; first 550 randomized patients)
- Secondary: Overall Survival (OS; all patients)
- Treatment arms:
- Cabozantinib 40 mg/day with nivolumab 3 mg/kg and ipilimumab 1 mg/kg intravenous (IV) every 3 weeks for 4 cycles, followed by nivolumab 480 mg IV every 4 weeks for up to 2 years
- Placebo with nivolumab 3 mg/kg and ipilimumab 1 mg/kg intravenous (IV) every 3 weeks for 4 cycles, followed by nivolumab 480 mg IV every 4 weeks for up to 2 years
- Results:
- Median follow-up time: 45 months
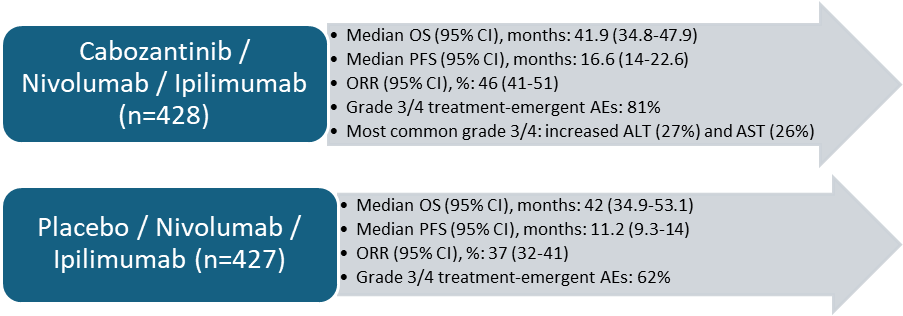
- Abbreviations: AE = adverse events, CI = confidence interval, ORR = overall response rate
- Important Takeaways:
- First-line treatment with triple therapy continues to demonstrate PFS and ORR benefit in patients with intermediate or poor risk with comparable OS between the 2 arms
- Higher grade 3/4 treatment-emergent AEs with triple therapy
What is KIM-1?
- A type 1 transmembrane protein that is primarily expressed in the proximal tubules of the kidneys in response to injuryPlays a critical role in the repair of renal tubular cells following damageElevated levels in the bloodstream or urine are often associated with kidney injury, including conditions like acute kidney injury (AKI) and RCCThe KIM-1 ectodomain is detectable in plasma and serumKIM-1 has been shown to be overexpressed in RCCSignificant findings:
- Evaluation of circulating kidney injury marker-1 (KIM-1) as a prognostic and predictive biomarker in advanced renal cell carcinoma (aRCC)
- Key Question: Are KIM-1 levels at baseline and after 1 cycle of nivolumab + ipilimumab or sunitinib associated with treatment outcomes?Key Findings:
- Higher levels of KIM-1 at baseline were associated with shorter overall survival (OS) independent of International Metastatic RCC Database Consortium (IMDC) risk group, nephrectomy status and tumor burden, in both the nivolumab + ipilimumab and sunitinib armsDecrease in KIM-1 from baseline to Cycle 2, day 1 (3 weeks after Cycle 1, day 1) was strongly associated with progression free survival (PFS) and OS among patients treated with nivolumab + ipilimumab, but not in patients treated with sunitinibPatients with a >30% decrease in KIM-1 had a median PFS of 70.8 months versus 4.2 months for those with a >30% increase in KIM-1Median OS was 85.4 months versus 26.6 monthsOverall response rate (ORR) was 69.3% versus 13.9%
- Circulating KIM-1 may be a useful minimally invasive biomarker for monitoring patients on RCC immunotherapy
- Key Question: Does kidney disease, a common co-morbidity among RCC patients, impact the association of KIM-1 with RCC outcomes?Key Findings:
- Higher baseline levels of KIM-1 were associated with worse progression-free survival and overall survival in patients with metastatic renal cell carcinoma.Plasma KIM-1 remained a significant prognostic marker for PFS and OS even after adjusting for other kidney injury biomarkers (cystatin C, TNFR1, TNFR2) and estimated glomerular filtration rate (eGFR).The prognostic value of KIM-1 was consistent across clear cell and papillary RCC.KIM-1 proved more prognostic for OS outcomes than the IMDC risk groups.
- The prognostic value holds true even in patients who have coexisting acute kidney injury (AKI) or chronic kidney disease (CKD).The addition of KIM-1 improves IMDC model performance and may be useful for risk prognostication in RCC
- Key Question: Are KIM-1 levels at baseline and after 1 cycle of nivolumab + ipilimumab or sunitinib associated with treatment outcomes?Key Findings:
- Evaluation of circulating kidney injury marker-1 (KIM-1) as a prognostic and predictive biomarker in advanced renal cell carcinoma (aRCC)
- Important Takeaway:
- Promising findings, but additional studies needed to prospectively validate the utility of KIM-1 as a biomarker for RCC
- Learn More
- 651 patients, median follow up of 67.6 months (5.5 years)
- Tx arms: nivolumab + cabozantinib (NC) vs sunitnib (S)
- Updated results:
- Median PFS: 16.4 months (NC) vs 8.3 months (S)
- 42% reduction in the risk of disease progression of death (HR 0.58, 95% CI [0.49, 0.7])
- Median OS: 46 months (NC) vs 35.5 months (S)
- 21% reduction in the risk of death (HR 0.79, 95% CI [0.65, 0.96])
- ORR: 55.7% (NC) vs 27.4% (S)
- Median duration of response: 22 months (NC) vs 15.2 months (S)
- Median PFS: 16.4 months (NC) vs 8.3 months (S)
- Important Takeaways:
- Long-term efficacy observed with combination nivolumab plus cabozantinib vs sunitinib
- Safety and tolerability were management and consistent with previously reported results
- Continued support for utilization of combination nivolumab plus cabozantinib as standard of care
- Study Population:
- 1167 respondents to online survey with 492 receiving systemic therapy for mRCC
- Therapy line: 42% first, 30% second, 13% third and 15% fourth or higher
- Findings:
- Hospitalizations and visits to the emergency room were significantly correlated with lower quality of life (QOL) and higher NCCN distress score (p<.001)
- 89% of patients think about cancer every day; 44% spend a few to several hours per day thinking about cancer
- mRCC affects activities of daily living (eating and sleeping) and ability to socialize
- Important Takeaways:
- Patients with mRCC need streamlined care (clinic, lab, ER visits) to minimize burden of cancer and improve QOL
- Important to assess both physical and mental impact of cancer for patients (and caregivers) and promote programs to improve support and QOL
- HC-7366 is a novel, highly selective and potent activator of general control nondepressible 2 (GCN2) kinase
- Novel mechanism of action:
- GCN2 kinase is a core regulator of metabolic stress through activation of the integrated stress response, where prolonged activation suppresses protein synthesis and induced cell cycle arrest, ultimately leading to apoptosis
- HC-7366 decreases HIF expression in tumor and immunosuppressive myeloid cells, inhibiting glycolysis, oxidative phosphorylation, and TCA cycle function in tumor cells
- Trial design:
- Treatment arms include HC-7366 60 mg daily monotherapy or HC-7366 (20 mg, 40 mg, 60 mg daily) in combination with belzutifan 120 mg daily
- Secondary endpoints include ORR, duration of response (DOR), time to response (TTR), disease control rate (DCR), PFS, and OS
- Key inclusion criteria include prior therapies, >/= 1 measurable lesion, and willingness to provide biopsy or archival tumor samples at two timepoints
- Important Takeaway:
- Future directions to follow up on the results of this novel mechanism of action for potential use in RCC
- Data regarding the use of treatment among 70-year-old or older patients are scarce
- CABOLD study seeks to address these gaps by addressing the real-life use of combinations in older patients
- Trial design:
- Patients will receive standard of care treatment consisting of cabozantinib 20 mg or 40 mg daily and nivolumab on a 28-day cycle (240 mg on Days 1 and 15 for the first 2 cycles, followed by 480 mg on Day 1 for subsequent cycles)
- Patients will benefit of a multi-modal follow-up including medical oncologists, geriatricians, and trained nurses to monitor safety closely
- Primary endpoint is to describe real-life treatment patterns of cabozantinib and nivolumab including dose modifications and interruptions due to toxicity
- Secondary endpoints include efficacy, survival, tolerance, and quality of life
- Important Takeaway:
- Future directions to follow up on the results of combination of cabozantinib and nivolumab among older patients with RCC
- Background:
- A benign solid tumor of the kidney
- Patients do not experience noticeable symptoms that prompts a workup
- Symptomatic tumors may cause flank pain, hematuria, or retroperitoneal bleeding
- Usually found incidentally through imaging that patients may undergo for other clinical reasons
- Due to the benign nature, usually monitored without any acute intervention or treatment until they reach 4-6 centimeters; they then may be treated based on clinical judgement and symptom presentation
- Study Population:
- 839 patients, about 82% were female with a median age of 59 years
- Findings:
- Patients with bleeding were noted to have larger tumors (6.5cm) on initial imaging compared to patients that did not report bleeding were noted to have smaller tumors (1.2cm or less)
- There are significant differences in characteristics and growth patterns between patients that experienced bleeding and those that did not
- Important Takeaway:
- Patients with larger tumor growth experienced greater bleeding and change in tumor size compared to patients that did not report bleeding, which was a significant factor in determining course of intervention
- Advanced or metastatic RCC patients were randomized 1:1 to receive nivolumab 1200 mg SQ + recombinant human hyaluronidase PH20 every 4 weeks or nivolumab 3 mg/kg IV every 2 weeks until disease progression
- SQ administration given over 2-8 minutes in the thigh or abdomen
- After 8 months of minimum follow-up, ORR was 24.2% with nivolumab SQ (95% CI 19-30%) vs 18.2% with IV nivolumab [95% CI 13.6%-23.6%; relative risk 1.33 (95% CI 0.94-1.87)]
- Nivolumab SQ was noninferior to nivolumab IV based on PK and ORR without any new safety signals being observed
- Important Takeaway:
- SQ nivolumab may be coming to your clinic soon!
- Background:
- Clear cell renal cell carcinomas are associated with VHL gene inactivation, like what is found in von-Hippel-Lindau disease, a genetic disorder
- This causes the activation of the transcription factor hypoxia-inducible factor 2α (HIF-2α), leading to a hypoxic state that drives angiogenesis and tumor growth and proliferation
- Belzutifan specifics:
- A pill that is used in the treatment of advanced kidney cancer
- Approved by the FDA in 2021 for the treatment of VHL and in 2023 for clear cell RCC based on the Litespark-005 clinical trial
- Blocks HIF-2α from interaction with other regulators in the cellular hypoxic state and diminishes the availability of targets for tumor growth
- Standard dose is 120 mg (40 mg tablets) taken by mouth daily
- Generally well tolerated:
- Side effects are anemia, shortness of breath, fatigue, mild nausea, and/or muscle aches
- It can be administered with or without food
- Important Takeaway:
- It continues to be studied with other medications as part of clinical trials to assess its effectiveness in treating renal cell carcinoma
Learn something new today? Be sure to share this write-up with your colleagues!
A special thanks to our CAB members who provided these reviews: Julia Batten, Jan Jackson, Nancy Moldawer, Virginia Seery, and Emily Wang!
The post Kidney Cancer Research Updates for the Entire Clinical Team appeared first on Kidney Cancer Association.
Adolescent & Young Adult (AYA) Cancer Awareness Week 1 Apr 1:02 AM (27 days ago)
On average, someone who receives a kidney cancer diagnosis is in their 60s. However, kidney cancer can affect children, adolescents, and adults of any age. That means an unthinkable and all-consuming life event hits just when someone should be engrossed in school, their career, and building families and communities. We’re recognizing Adolescent & Young Adult Cancer Awareness Week by sharing stories from young people who navigated the practical realities and emotional roller coaster of a kidney cancer diagnosis.

The post Adolescent & Young Adult (AYA) Cancer Awareness Week appeared first on Kidney Cancer Association.
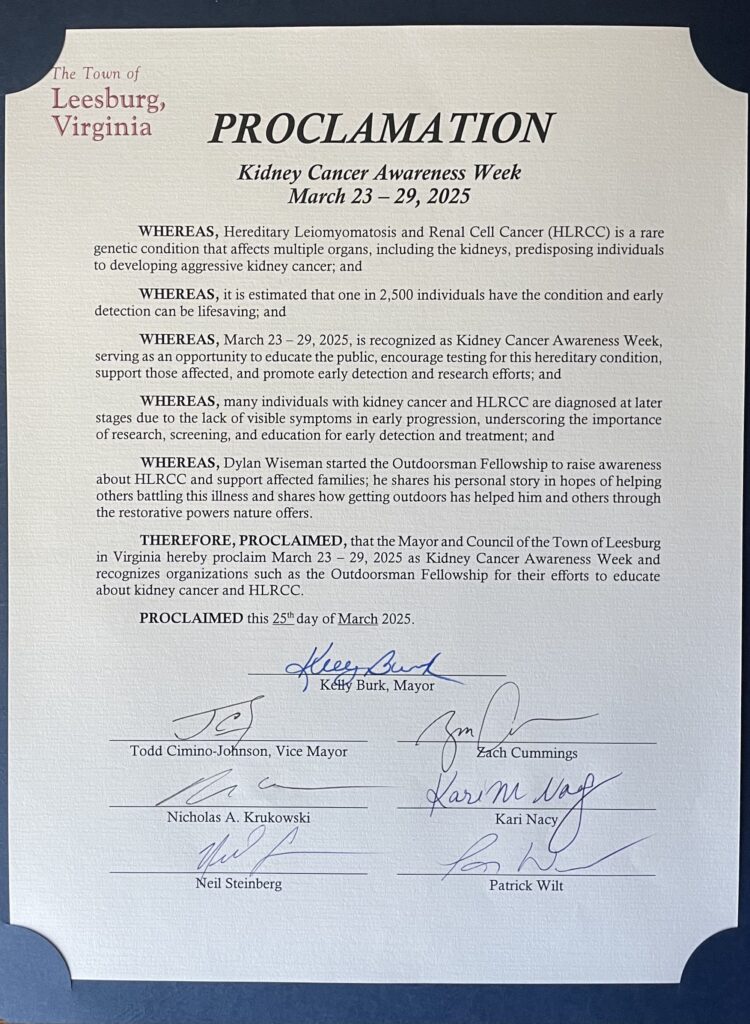
The Outdoors Nurtured Dylan Through Kidney Cancer 28 Mar 6:36 AM (last month)
This is a guest post by Dylan Wisman, 28, of Winchester, VA.

My name is Dylan Wisman, and in November 2023, my life changed forever. I was 27 and back in Missouri for an alumni wrestling weekend — but just as importantly, I was out deer hunting, chasing another elusive Missouri wall hanger. That Friday morning, out in the woods and more than half a mile from my car, I noticed blood in my urine and started experiencing intense side pain. Thirty minutes from the nearest urgent care, I tried to convince myself it wasn’t serious. After all, I had just been hiking through Olympic National Park, Mount Rainier, and the North Cascades a few weeks earlier. I felt strong and healthy.
A couple of weeks later, back home in Virginia, I was diagnosed with stage 3 kidney cancer. Genetic testing revealed I have HLRCC (Hereditary Leiomyomatosis and Renal Cell Cancer), a rare genetic condition that increases the risk of developing aggressive kidney cancer. At 27 years old, I didn’t fully understand what any of it meant — only that I suddenly had cancer, and it was serious.
In February, doctors removed my kidney. I’m no stranger to surgery and recovery — my college wrestling career was built around pushing through injuries. But this was different. After surgery, they told me they found a tumor on my vena cava, the main vein leading to the heart. It was inoperable. We regrouped, did full-body scans, and in May, I got the news no one wants to hear: the cancer had spread. My stage 3 diagnosis had turned to stage 4. It was now in my lungs, liver, spleen, pelvis, spine, shoulder — and a large mass had grown near where my kidney had been.
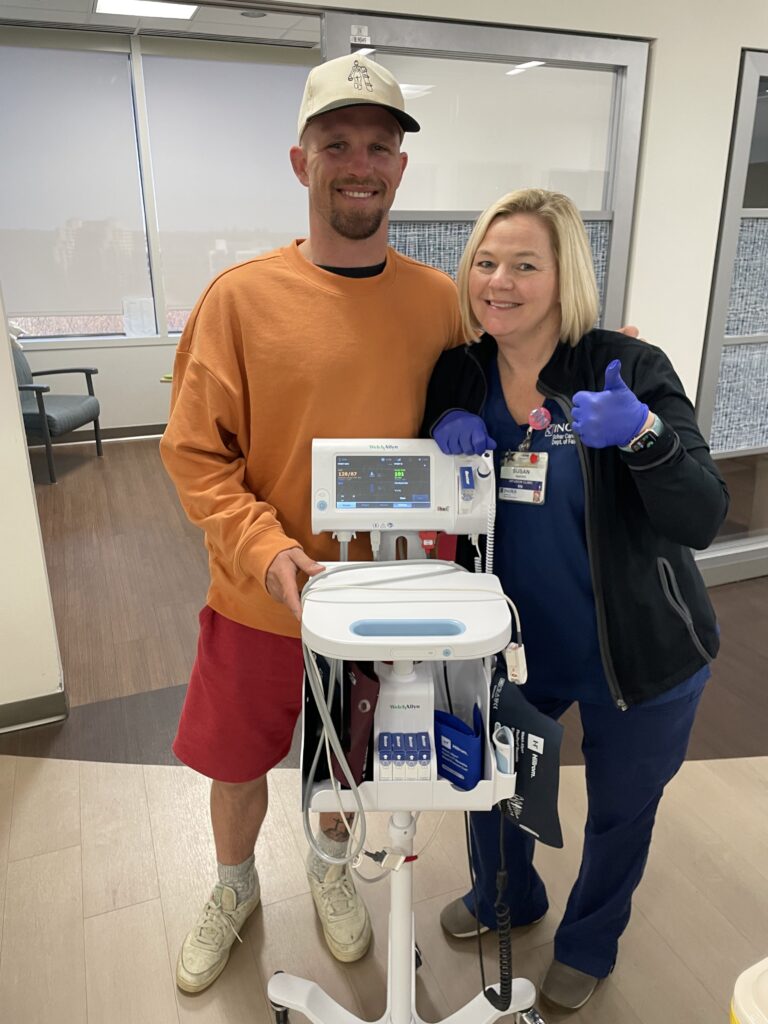

Treatment began, and it got worse before it got better. In those darkest moments, I turned to the only therapy I knew: nature.
Whenever I could, I dragged myself outside — into the woods, onto the water, or just preparing for the next hunting season. Nature has always been my escape. Hunting, fishing, hiking — those moments have shaped me. There’s a peace, a purpose, and a camaraderie that comes with being outdoors. You have to experience it to really understand it. For me, it’s always been where I feel most alive.
That connection is what inspired me to start The Outdoorsman Fellowship, a nonprofit dedicated to spreading awareness, promoting genetic testing, and funding kidney cancer research. But even more than that, it’s about reminding people — especially those going through their own battles — that nature is God’s greatest creation, and we all have access to its healing power in one form or another.
Yes, this story is about me, but the mission is bigger. I want to advocate for others going through tough times and remind them they’re not alone.
What I’ve Learned
If you’re going through something similar, here’s what I want you to know:
- Find joy. Smile, do what makes you happy, and surround yourself with things that bring you peace. Your mindset is more powerful than any treatment.
- Be your own advocate. Don’t wait for someone else to fight for you. Ask questions, speak up, and make sure you’re being heard.
- Never give up. Cancer is just another obstacle — and obstacles are meant to be overcome.
- You are not alone. There are people who care and want to help. Let them in.
- Stay on top of your health. Even if you feel fine, make those yearly checkups a priority. If something feels off, get it checked out.

This journey has opened my eyes and changed the way I see life, strength, and community. If you’re in your own fight, know this — you don’t have to do it alone.
The post The Outdoors Nurtured Dylan Through Kidney Cancer appeared first on Kidney Cancer Association.
Why We Must Restore Funding for the CDMRP 27 Mar 5:09 AM (last month)
The Congressionally Directed Medical Research Programs (CDMRP) was created by Congress in 1992 to fund high-impact medical research—especially in areas overlooked by traditional sources—through the Department of Defense. CDMRP began with breast cancer research and has since expanded to support many conditions affecting both Service Members and civilians.
The CDMRP’s unique strength lies in backing high-risk, high-reward science: early-stage, innovative ideas that can lead to major breakthroughs but often don’t qualify for NIH funding.
Over the years, CDMRP has enabled progress in immunotherapy, post-traumatic stress disorder (PTSD) treatment, traumatic brain injury recovery, and rare diseases. It funds projects that fill research gaps and includes patient advocates in decision-making to ensure the research goals align with patient needs.
Importantly, since 2017, the CDMRP has had a dedicated Kidney Cancer Research Program (KCRP) – a direct result of consistent, vocal advocacy from patients, families, health care professionals, and advocacy organizations. And because we continued advocating, what began as a $10 million program grew to a $50 million program. We had hopes of seeing the KCRP grow to $60 million in the near future.
This progress has come to a halt. In the most recent continuing resolution to fund the federal government for 2025, Congress cut funding for the KCRP $50 million to $0, and overall CDMRP funding was reduced by 57%.
Impact in Action
One powerful example of CDMRP’s impact is Dr. Pavlos Msaouel’s research on renal medullary carcinoma (RMC)—a rare, aggressive kidney cancer primarily affecting young African Americans with sickle cell trait, including Service Members. Before his work, RMC had no known risk factors and a grim prognosis.
Initial funding from the KCA allowed Dr. Msaouel to research RMC specifically. In 2018, Dr. Msaouel received a CDMRP KCRP Concept Award that allowed him to explore an innovative idea: could intense exercise or dehydration trigger kidney damage in people with sickle cell trait? Using mouse models, his team showed that exercise-induced hypoxia caused red blood cell sickling and tissue damage in the kidney’s inner medulla, particularly on the right side due to lower blood flow—which also might explain why RMC often occurs in the right kidney.
These early findings—funded by CDMRP—led to additional grants from the KCA and to a follow-up clinical study supported by the National Cancer Institute, confirming the link between high-intensity physical activity and increased RMC risk in human patients. This was the first modifiable risk factor identified for RMC. It now guides physicians in counseling patients with sickle cell trait—potentially preventing RMC or catching it earlier.
Compared to the prognosis for RMC patients just 5 years ago, Dr. Msaouel’s research has resulted in improved survival in many and eradication of disease – meaning they are cured – in about 5-10% of his patients.
Without CDMRP, this research might never have happened. Promising new treatments now entering clinical trials with the potential to cure cancer could be delayed—or lost altogether. CDMRP isn’t redundant; it’s irreplaceable. It backs research NIH or other programs may not be able to currently fund. It empowers patient-centered innovation. And it saves lives.
Congress must reverse the decision to eliminate this funding. Patients—and progress—depend on it.
The post Why We Must Restore Funding for the CDMRP appeared first on Kidney Cancer Association.
In His Memory: Lessons from my Father’s Battle 26 Mar 10:54 PM (last month)
This is a guest post by Kiana Jones. Kiana’s father Sammie Jones was diagnosed with kidney cancer and passed away in 2024.

My father, Sammie Jones, was more than a cancer patient; he was a loving husband, father, and grandfather who wanted to live and fight to be with his family. My dad was a farmer for 51 years and a lover of hunting, fishing, and spinning records as “DJ Hunter.” He was a devoted husband, father, and grandfather whose laughter and kindness lit up every room.
On November 21, 2021, my father was diagnosed with prostate cancer. Thankfully, it was caught early, and he began radiation therapy immediately. After completing treatment in 2022, he believed the cancer was gone. However, during his annual check-up in May 2024, we discovered it had returned. Around the same time, a spot was detected on his right kidney, delaying further radiation. In July, he was diagnosed with kidney cancer, and his doctor at University of Mississippi Medical Center recommended surgery to remove the kidney and begin chemotherapy. Unfortunately, and despite us advocating for it, the surgery didn’t happen.
Sadly, his health declined rapidly and by October 2024 he lost mobility in his legs, and further tests revealed the cancer had spread to his left kidney, spinal cord, lungs, and ribs, making surgery too risky at that point. In the ICU, my father battled fluid on his lungs, breathing difficulties, and kidney failure. He was placed on a ventilator, oxygen, and dialysis. On November 21, 2024, exactly three years after his initial diagnosis, he passed away.
Going through this process, especially knowing it would eventually lead to saying goodbye, taught me so much about love, resilience, and the importance of being present.
One of the key things we learned was how vital it is to cherish every moment, no matter how small. Even in the midst of challenges, there were moments of connection and joy that became deeply meaningful.
For our family, this experience was both heartbreaking and unifying. We leaned on each other in ways we hadn’t before, finding strength in shared memories and mutual support. Practical help from friends and extended family—like meals, errands, or simply sitting with us—was invaluable. Spiritually, we found comfort in reflecting on his life and the legacy he left behind. Rituals, whether religious or personal, helped us process our grief and celebrate his memory.
Cherish the moments that matter, no matter how small
For anyone facing something similar, I would want them to know that it’s okay to feel overwhelmed, scared, or uncertain—those emotions are natural. What matters most is taking things one step at a time and remembering that you don’t have to go through it alone. Lean on your support system, whether it’s family, friends, or even support groups, and don’t hesitate to ask for help when you need it.
Advocating for yourself or your loved one is crucial. Stay informed, ask questions, and trust your instincts when it comes to decisions about care and treatment. If something doesn’t feel right, seek a second opinion or push for clarity.
Also, cherish the moments that matter, no matter how small. Even in difficult times, there can be opportunities for connection, laughter, and love, and those moments can provide strength.
Finally, self-compassion is vital. It’s easy to feel like you should have all the answers or do everything perfectly, but you’re human, and it’s okay to take breaks, feel vulnerable, and lean into the process of healing and coping. You’re stronger than you know, and there’s a community of people ready to support you.
The post In His Memory: Lessons from my Father’s Battle appeared first on Kidney Cancer Association.
What’s New in Kidney Cancer Research 18 Mar 10:07 AM (last month)

Welcome back to our blog series about kidney cancer clinical trials where we break down recent research into key updates for patients and others interested in advances in the field from the major cancer conferences including the 2024 American Society of Clinical Oncology’s (ASCO) annual meeting, the 2024 European Society for Medical Oncology (ESMO) annual meeting, the 2025 ASCO genitourinary focus meeting (ASCO GU), as well as the Kidney Cancer Association’s own International Kidney Cancer Symposiums (IKCS).
While 2024 was somewhat quiet in terms of groundbreaking kidney cancer advancements, research remains incredibly active with several promising findings.
Since January 1, 2024, an impressive 79 new clinical trials have opened and currently enrolling, a testament to the relentless pursuit of better treatments. Although we’re still waiting for that definitive cure, there are some good, less good news, and exciting concepts to share. As we did in our first blog, we will highlight some terms along the way to help you decode some of the clinical trial language and try to highlight for each study why this is important. So, without further ado, let’s dive deeper into the most intriguing developments since our last review in May 2024.
One highly anticipated trial, SUNNIFORECAST, was showcased at ESMO 2024. This study was important because it evaluated, for the first time, the efficacy of immunotherapy—specifically the combination of ipilimumab and nivolumab (IPI-NIVO)—for patients with non-clear cell renal cell carcinoma (nccRCC). Historically, nccRCC subtypes have been underrepresented in kidney cancer research, receiving far less attention compared to clear cell RCC (ccRCC), and this was the first study that enrolled over 300 nccRCC patients.
The results were remarkable and encouraging. Patients receiving IPI-NIVO experienced significantly improved survival rates. Specifically, the combination increased the one-year overall survival (OS) rate to 86.9%, compared to 76.8% with standard treatments, a notable advancement for these underserved patient groups. The median OS also improved dramatically from 33.9 months to 42.4 months. While progression-free survival (PFS) was similar between groups, the overall response rate, indicating tumor shrinkage, was considerably better at 32.8% compared to just 19.6% in patients receiving traditional therapies.
Interestingly, sub-analyses showed that patients whose tumors expressed the biomarker PD-L1 protein and those with lymph node metastases benefited even more, highlighting potential patient-specific markers that might predict treatment success. Among various nccRCC subtypes, patients with papillary and non-papillary RCC showed the most improvement. However, the chromophobe RCC subgroup gained less benefit, emphasizing the need for more targeted research within these specific subtypes. Despite the numbers telling a clear story of a meaningful shift towards better survival, the fact that the nccRCC population included a complex mix of different histology and standard treatments in the control group, interpreting the results has raised quite a debate among experts that would like to see more studies like SUNNIFORECAST that could answer more precise questions for specific kidney cancer subtypes.
Decoding clinical trials:
Different histology: Refers to the various microscopic structures and subtypes of cancer cells observed in tumors. Recognizing different histologies helps doctors tailor specific treatments, as not all kidney cancers respond similarly to the same therapies.
Biomarker: A biological indicator measurable in blood, tissue, or body fluids, which can help doctors predict treatment responses, disease progression, or prognosis, guiding more personalized medical decisions.
Another eagerly awaited study, TiNivo-2, also reported findings at ESMO 2024. It tested the combination of tivozanib, an approved tyrosine kinase inhibitor (TKI)—a drug that blocks enzymes responsible for cancer cell growth—with nivolumab, a checkpoint inhibitor immunotherapy, against tivozanib alone. The scientific community was keenly interested to determine if adding immunotherapy could further improve patient outcomes, especially in cases previously treated with immunotherapy, a strategy known as immunotherapy rechallenge.
Contrary to expectations, this combination did not yield significantly better results. The median progression-free survival was similar in both groups, indicating no substantial advantage to adding nivolumab to tivozanib. Preliminary overall survival data also suggested minimal differences between groups, highlighting that single-agent tivozanib remains effective, particularly as a well-tolerated later-stage therapy. Patients also experienced more side effects when combining these two drugs, underscoring the importance of evaluating the benefit-risk balance in treatment decisions. This insight provides valuable guidance on the limitations of immunotherapy rechallenge in certain patient groups.
Decoding clinical trials:
Tyrosine kinase inhibitor (TKI): A targeted cancer treatment that blocks specific enzymes (tyrosine kinases) involved in cancer cell growth, blood vessel formation, and tumor spread. TKIs are commonly used in advanced kidney cancer.
Immunotherapy rechallenge: Trying immunotherapy treatment again after previously receiving it. This approach investigates whether patients can benefit from another round of immunotherapy, especially when combined with other drugs.
Understanding biomarkers to predict treatment response remains one of kidney cancer research’s greatest challenges. Exciting progress was presented at ASCO GU 2025 through the CheckMate 214 trial, investigating kidney injury marker-1 (KIM-1) as a potential predictive biomarker. KIM-1, detectable in blood samples, has previously been linked to kidney cancer prognosis. Researchers measured KIM-1 levels before and after initiating nivolumab and ipilimumab therapy, observing astonishing outcomes.
Patients with a significant decrease (over 30%) in KIM-1 after a single treatment cycle experienced dramatically improved outcomes, achieving median progression-free survival of 70.8 months compared to just 4.2 months in those whose KIM-1 levels increased significantly. Similarly, overall survival was substantially better at 85.4 months versus 26.6 months. These compelling findings position KIM-1 as a highly promising biomarker, potentially revolutionizing how doctors personalize treatment and helping patients avoid ineffective therapies.
Further good news emerged from ASCO GU 2025, where the COSMIC-313 trial provided key updates on a triple therapy combination: cabozantinib, nivolumab, and ipilimumab (C+N+I). This potent regimen significantly improved progression-free survival to 16.6 months compared to 11.2 months with nivolumab and ipilimumab alone. Response rates also notably increased, offering robust proof of the combination’s effectiveness. Despite these gains, overall survival remained comparable between groups, highlighting the continued necessity for further research and refinement in treatment strategies. Nonetheless, COSMIC-313’s manageable safety profile makes this triple combination an appealing and viable treatment option for advanced RCC patients, enhancing their quality of life by significantly delaying disease progression.
CheckMate 9ER also delivered reassuring long-term outcomes for nivolumab plus cabozantinib at ASCO GU 2025, firmly establishing this combination as a leading therapy in advanced RCC. Patients benefited greatly, experiencing substantial improvements in progression-free survival (16.4 months versus 8.3 months) and overall survival (46.5 months versus 35.5 months) compared to standard sunitinib treatment, alongside significantly better response rates. This study underscores the durability and effectiveness of the nivolumab-cabozantinib regimen.
Read more about ASCO GU 2025 here.
Finally, we turn to a promising newcomer, Casdatifan, a novel HIF-2α inhibitor. At ASCO 2025, researchers presented encouraging results from the ARC-20 study in patients whose cancers progressed despite previous treatments. Casdatifan demonstrated a 34% tumor shrinkage rate in patients receiving higher doses, with particularly notable benefits in those classified with favorable risk factors, meaning patients with certain clinical characteristics known to indicate better outcomes. The drug was generally well-tolerated, with manageable side effects such as mild anemia and occasional low oxygen levels.
Decoding clinical trials:
Tyrosine kinase inhibitor (TKI): A targeted cancer treatment that blocks specific enzymes (tyrosine kinases) involved in cancer cell growth, blood vessel formation, and tumor spread. TKIs are commonly used in advanced kidney cancer.
Immunotherapy rechallenge: Trying immunotherapy treatment again after previously receiving it. This approach investigates whether patients can benefit from another round of immunotherapy, especially when combined with other drugs.
You may wonder why this is exciting, especially since belzutifan is an approved drug with the same mechanism of action. Well, having Casdatifan or any other drug as an alternative to the only available option on the market could bring several advantages for patients, including an expanded spectrum of efficacy due to differences in how the drugs work, a potentially different side effect profile for some patients, and most importantly, reducing financial toxicity. Having multiple drugs in the same class can lead to better competition, potentially lowering costs and improving insurance coverage, making treatment more accessible to those in need.
Exciting New Trials on the Horizon
An ongoing trial ( Clinical Trial NCT06318871) is testing an innovative approach using cytokine-induced memory-like (CIML) natural killer (NK) cells. Unlike traditional therapies, this trial introduces a new immune-based strategy that differs from chimeric antigen receptor T-cell (CAR-T) cell therapy, which has struggled to treat solid tumors like kidney cancer.
Decoding clinical trials:
CIML NK cells (Cytokine-Induced Memory-like Natural Killer cells): A special type of NK cells enhanced with cytokines to boost their natural cancer-fighting abilities, making them potentially more effective in targeting and destroying cancer cells in kidney cancer treatment.
CAR-T (Chimeric Antigen Receptor T-cell therapy): A personalized immunotherapy that involves modifying a patient’s own T-cells (a type of immune cell) to better recognize and attack cancer cells. Although successful in certain blood cancers, CAR-T therapy is still being studied for its potential effectiveness against solid tumors, including kidney cancer.
CAR-T therapy has transformed blood cancer treatment but faces challenges in solid tumors due to the tumor’s harsh environment. This trial takes a different approach, enhancing NK cells with cytokines to boost their cancer-fighting ability before reintroducing them into the patient. Unlike CAR-T, this method is designed to be more accessible, scalable, and potentially safer for advanced RCC patients.
This is the first time CIML NK cells are being tested in combination with low-dose IL-2, a cytokine that activates immune cells, in patients with advanced clear cell renal cell carcinoma and urothelial carcinoma.
This breakthrough was made possible by a 2021 Kidney Cancer Association Research Award to Dr. Toni Choueiri and Dr. Rizwan Romee at the Dana-Farber Cancer Institute, which helped move this concept from research to clinical testing. If successful, this therapy could provide a new option for patients who have exhausted other treatments, potentially improving survival and quality of life. Trials like this represent the future of cancer care—more precise, innovative, and patient-focused. Read an update about this research HERE.
How to Stay Informed and Get Involved
I hope this update helped enrich your understanding of new kidney cancer research – please share your thoughts with us! Staying informed and potentially getting involved in clinical trials can be a pivotal part of navigating your kidney cancer journey. Patients and caregivers play a pivotal role in the success of clinical trials. By participating, you contribute to the advancement of medical knowledge and help future patients receive better care. If you’re considering joining a trial, we encourage discussing it with your healthcare provider to understand how it might fit into your treatment plan.
Additional Resources:
The post What’s New in Kidney Cancer Research appeared first on Kidney Cancer Association.